Prostate disease is one of the most common and insidious in men over 40 years of age. At first, patients may not even know the presence of the problem, but over time, the symptoms will make themselves feel. If you do not see a doctor in time, prostatitis becomes chronic and complications can occur. Depending on the severity, causes, and nature of the course, different types of prostatitis are distinguished.
Types of prostatitis according to the form of the course:
- acute;
- chronic;
- hidden.
What is prostatitis due to the occurrence of:
- herpetic;
- bacterial;
- calculus;
- pangó;
- infectious;
- purulent;
- chlamydial;
- fungal;
- gonorrhealis;
- fibrous.
Classification
Faced with an unpleasant disease of the urogenital system such as inflammation of the prostate gland, many men wonder why they have prostatitis.
Understanding the etiology of the disease will help in accurate diagnosis and effective prevention.
According to the form of flow
According to the form of the course, prostatitis is divided into acute, chronic and latent, between which catarrhal, follicular, parenchymal (purulent) symptoms are distinguished.
The disease has the following forms:
- With catarrhal prostatitis in the male body, urinary incontinence and discomfort occur in the pubic region. This is the most common type of acute prostatitis.
- Follicular prostatitis is characterized by symptoms such as lumbar or rectal pain, fever, and severe urinary incontinence (dysuria). In a more advanced form, when the patient postpones a visit to the doctor, urinary pain occurs during urination and urinary retention occurs.
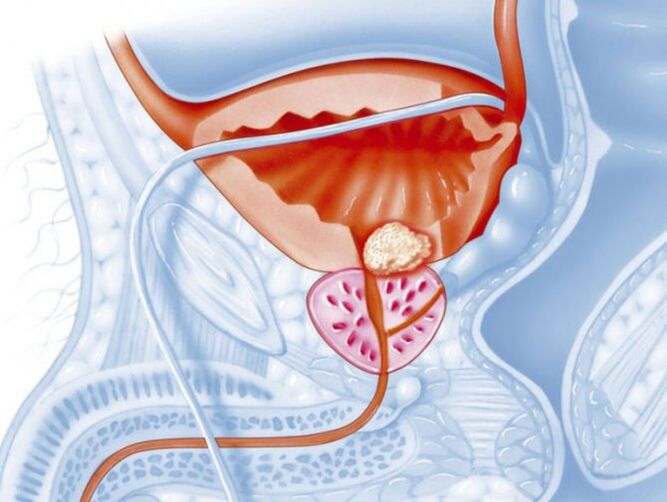
- Parenchymal prostatitis - an abscess containing pus that forms in the body of the prostate gland. In this case, fever occurs, sharp pains appear with frequent urination stimuli. The temperature rises to 39-40 ° C, defecation becomes almost impossible.
Acute prostatitis
Acute prostatitis is a condition in which inflammation of the prostate gland occurs over a short period of time and is characterized by a variety of symptoms. Swelling of the gland occurs, which is provoked by the negative effects of the pathogenic microflora. Disease-causing bacteria disrupt tissue integrity, causing constant discomfort in the pelvic region, even at rest.
There are several dominant ways for infection to enter the prostate gland:
- with inflammation of the rectum - the lymphogenic pathway;
- after infectious diseases - hematogenous;
- directly through the urethra - ducted.
Excessive accumulation of prostate content creates excellent conditions for bacteria to multiply, which causes various complications:
- abscess;
- BPH;
- prostate cancer;
- loss of potency;
- infertility.
The symptoms of prostatitis are so painful that the patient is forced to see a doctor urgently for help. If you don’t do this in time, prostatitis becomes a chronic form that is much harder to cure. Antibiotic therapy in combination with immune-boosting drugs is effective in fighting the disease.
Chronic prostatitis
Symptoms of chronic prostatitis are usually found in the background of congestion of the prostate gland caused by an untreated disease in acute form. It usually occurs in men over the age of 50 who did not seek help and self-healed. In many of these cases, complications developed due to concomitant diseases. In addition, not everyone is sexually active enough at this age, as a result of which the secret thickens and stagnates in the prostate, leading to dysfunction. Interrupted intercourse also triggers fluid stagnation. According to modern research, about 40% of people who experience symptoms of chronic prostatitis experience erectile problems.
Chronic prostatitis usually has mild symptoms that only appear when it gets worse. Patients experience dull pain in the groin area, which intensifies after physical exertion and at the end of the day. Often the pain radiates to the lower back, scrotum, and perineum. Frequent urination is observed, especially at night, the stream flows intermittently, curves.
The sexual intercourse becomes shorter, an incomplete erection is detected, and sometimes there is pain in the vagina. Infertility is usually seen in people with chronic prostatitis, and impotence is virtually absent at this stage of the disease. Sometimes the color of the genitals changes, they turn purple due to improper blood circulation.
All symptoms of prostatitis get worse if left untreated. The condition is similar to manifestations of the acute course of the disease. Weakening of the immune system, stress, neglect of diet, bad habits - all this leads to worsening and worsening of the condition.
Often, the chronic form leads to the appearance of symptoms of diseases such as cystitis, kidney disease, and adenoma. The risk of developing urolithiasis and malignancy is increased. Often, the pathological process is almost asymptomatic and is accidentally discovered in laboratory tests related to another disease.
Because of the occurrence
There may be several reasons for the development of infectious and non-infectious etiology of prostatitis, as well as predisposing factors. Due to their incidence, the following types of prostatitis are distinguished:
- bacterial;
- calculus;
- pangó;
- infectious;
- purulent.
Sedentary lifestyle, frequent hypothermia, infrequent sexual activity, interrupted sexual intercourse, smoking, alcohol consumption, stressful situations - all these conditions affect the stagnation of secretions in the prostate gland and adjacent blood vessels. It can be divided into several forms depending on the causes of prostatitis.
Bacterial prostatitis
Bacterial prostatitis is caused by bacteria that enter the prostate in a variety of ways. It can be a kind of bacterium or a group of bacteria. The disease can be caused by:
- mushrooms;
- gonococcus;
- Koch's wand;
- chlamydia;
- several types of bacteria at once.
The inflammatory process is most often accompanied by the penetration of bacteria in the prostate caused by sexually transmitted diseases. Priority sex leads to diseases such as gonorrhea, chlamydia, fungal infections with frequent partner changes and the use of protective equipment. In addition, the development of pathology is facilitated by a decrease in immunity due to violation of the work and rest system. Bad habits such as smoking, alcohol consumption, sedentary lifestyle, etc. They also reduce immunity.
The most obvious symptoms that accompany bacterial prostatitis include cloudy discharge during burning, pain, and urination. The urine smells unpleasant. General symptoms associated with poisoning are: dizziness, weakness, nausea, fever. Pain is seen during ejaculation and sometimes blood is present. In chronic bacterial prostatitis, urination becomes more frequent, with yellowish or greenish discharge from the penis.
Calcular prostatitis
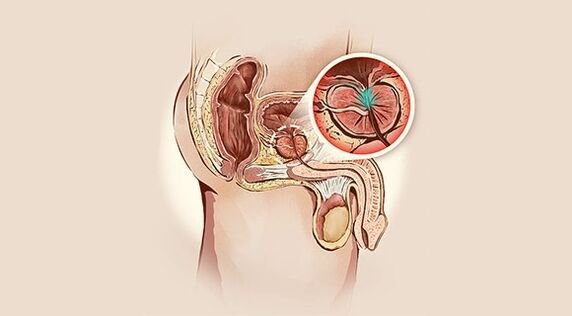
With calcular prostatitis, stones form in the channels of the prostate gland. This form of the disease is very complex and is accompanied by severe pain. The conglomerates are of different origins: phosphates, oxalates, predominantly calcium and protein.
There are two reasons for the occurrence of stones in the ducts: stagnation of gland contents and throwing urine into the prostate.
Stagnation is associated with various factors that interfere with the normal outflow of the selected fluid. Prolonged sexual abstinence, hyperplasia, the presence of a tumor-terminating tumor, and a sedentary lifestyle lead to stagnation of secretions and disruption of the vascular and lymphatic systems.

Urinary incontinence is caused by a malfunction of the sphincter that relaxes and urine flows both inside and out. The presence of stones and sand in the bladder contributes to the formation of stones in the channels of the prostate. They enter there with urine, settle down and continue to grow, eventually reducing the outflow. Genital injury and surgery can lead to sphincter dysfunction.
At first, the calculus form of prostatitis is asymptomatic as the stones grow, the symptoms appear and intensify. There is pain in the lower abdomen or scrotum that radiates to the buttocks and lower back. No resting pain is observed and occurs only during exercise, defecation and urination, and during intercourse and walking.
During their movement, large stones with sharp edges damage the canal, leading not only to pain but also to the release of blood in the urine and ejaculation. Stone wounds can easily become infected and then calcular prostatitis becomes contagious.
After about a month, in the case of calcular prostatitis, the work of the whole body is interrupted, the person feels unwell, experiences insomnia, increased fatigue and irritability.
In the advanced stage of calcular prostatitis, after a complete diagnostic examination, medication is prescribed and surgery is performed to remove the conglomerates.
Congestive prostatitis
The stagnant onset of prostatitis is due to a delay in the secretion of the prostate gland. Such problems are most commonly observed in men in sedentary work who do not engage in sports. As a result of hypodynamics, blood circulation in the pelvic organs is damaged, the prostate suffers from an insufficient supply of oxygen and nutrients, and stagnation and inflammation occur. If nothing is done, the disease becomes chronic and causes great discomfort.
Congestive prostatitis causes irregular sex or complete absence thereof. In this case, men should free the gland from the secretions on their own, but do not overdo it, as regular masturbation can be detrimental due to deficient ejaculation. Many spouses have found one way to prevent pregnancy, such as interrupted intercourse. It also leads to incomplete ejaculation and inflammation.

Sometimes hypothermia or varicose veins become a provocative factor. Disorders of the structure of the prostate gland can also cause stagnation. Regular overheating of the pelvic region and persistent constipation adversely affect secretion production. Depending on the factors that provoke the disease, several types of congestive prostatitis are distinguished.
- Venous prostatitis. It occurs in people with varicose veins of the lower extremities. In this disease, all the organs of the small pelvis are affected due to improper circulation.
- Congestive. It is formed by the partial emptying of the prostate gland. Gradual overflow leads to stagnation.
- Chronic. It develops when a bad lifestyle has become a habit. If nothing is done to change the situation, the disease becomes chronic. It is more common in single men with obesity, as early as adulthood, when they are burdened with a history of diseases. At this stage, the prostate often enlarges, which is easy to determine during the examination.
- Infectious. It connects to pre-existing inflammation of the prostate when the infection enters the urogenital system.
Manifestations of prostatitis include difficulty urinating, lumbar pain, tension during bowel movements, and decreased sexual activity. As a result of these symptoms, stagnant types of prostatitis develop poor health, irritability, reduced ability to work and disturbed sleep.
Infectious prostatitis
Microorganisms that cause signs of acute prostatitis include Escherichia coli, Staphylococcus aureus, Proteus, Eltirococcus, Klebsiella. There are bacteria that are constantly in the body but do not lead to inflammatory processes when sleeping. When it penetrates the mucous membrane of the prostate gland through the urethra, the process of development and multiplication of microorganisms begins, resulting in inflammation. Unsorted and unprotected sex also allows harmful bacteria to enter the body.
Typical symptoms are scrotum, perineum, lower abdomen, lower back, pelvic pain and burning sensation. Difficulty urinating, acute urinary retention. In addition to the listed symptoms that accompany the infectious type of prostatitis, constipation, urethral discharge, hemospermia, and pain during ejaculation may occur.
It is a dangerous disease that can trigger infection of a sexual partner at the earliest stages, leading to general sepsis or the development of pyelonephritis and cystitis.
Purulent prostatitis
Purulent prostatitis usually develops when a bacterial infection enters the prostate. The disease occurs in four stages.
- Catarrhal. Suffering from acute respiratory viral infections, tonsillitis, influenza. There is a purulent content in the urine. There is a burning sensation when the bladder is empty. Patients note a decrease in potency. The process that accompanies this type of prostatitis involves the surface tissues of the prostate.
- Focal. The process extends to the glandular tissue. The ducts swell and the outflow causes disturbance. The size of the gland increases due to the accumulation of pus that is excreted in the urine. Body temperature rises.
- Parenchymal. Connective tissue is involved in the process, the edema becomes even greater, the temperature can reach 40 ° C. The pain that erupted in the anus was accompanied by a false desire to defecate.
- Absolutely. It is the most insidious form of prostatitis. The temperature is severely disturbed, with plenty of pus and unbearable pain present. This stage can be complicated by peritonitis and is fatal.
Purulent prostatitis can be complicated by symptoms and diseases such as paraproctitis, paracystitis, abscess, sepsis. These pathologies are usually surgically treated and involve the removal of purulent sacs.
Diagnostics
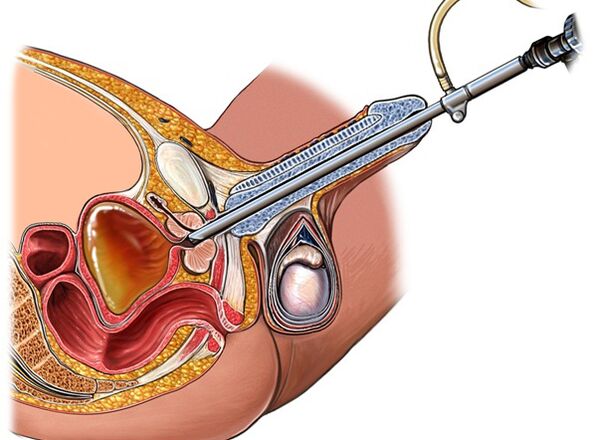
Diagnosing the types of prostatitis is not particularly difficult and begins with collecting a medical history to help you more accurately understand the picture of the disease. An rectal examination is then performed to determine the size of the gland, determine the nature of the pain, and reveal the presence of edema and seals.
In order to make a correct diagnosis, laboratory tests are prescribed:
- Analysis of urine;
- urine culture with AB susceptibility test
- general blood test;
- analysis of prostate secretion;
- blood chemistry;
- rectal examination.
Additional diagnostics include instrumental research methods. First, ultrasound is performed, if necessary, additional MRI and TRUS are prescribed. Relatively recently, a new PET screening method has emerged, which is considered to be the most informative.
Treatment of inflammation
Urologists treat all types of prostatitis. Traditional methods are good, but only with medical prescriptions and with the permission of the attending physician.
You need to find the cause of the disease first, and only then can you get post-symptomatic treatment.
- Active antibiotic therapy helps to cure prostatitis. Parenteral antibiotics are the most effective.
- Painkillers and diuretics appear with pronounced pain syndrome.
- In case of constipation, laxatives are prescribed.
- Novocaine blockade is placed with severe pain and difficulty urinating.
- We present the process of vitamin therapy and immune correctors.
- You may want to follow a special diet that excludes spicy, salty, smoked foods.
- Bed rest is required.
Among the local procedures, sitting baths with water whose temperature is two degrees higher than body temperature are presented. Enemas are made from a decoction of anti-inflammatory herbs with the addition of 1% anesthetic while the contents are slowly injected into the intestines and left there until the patient resists.
Physiotherapy treatment also has a beneficial effect in restoring prostate function. Massage of the prostate with acute prostatitis is prohibited, but is recommended in chronic form. UHF and a microwave are prescribed to restore normal circulation and alleviate edema to restore metabolism.
In case of prolonged urinary retention, a catheter is inserted. At some stages in the development of the disease, surgical treatment is indicated to open the purulent sacs by installing drainage.
Treatment of acute prostatitis takes several weeks to one month. In general, a favorable result is observed. If the disease has become more complicated or has entered a chronic stage, the process can be difficult, long, and can take several months.
Restrictions on sexual activity and the use of personal protective equipment are recommended during treatment.
The medical physiotherapy device helps to cure prostatitis. It effectively eliminates the symptoms of prostatitis, is able to restore decreased sexual activity, relieves pain, relieves swelling and inflammation. The device can be used both at home to treat and prevent diseases of the pelvic organs.
The device relieves muscle tension, improves sperm production, strengthens blood vessels and prevents other possible diseases in the small pelvis. The device, which is used to treat prostatitis in men, is equipped with an easy-to-use, heating and vibration mode controller and is powered from the mains. The compact size allows the device to be used in any conditions.
How to prevent the development of the disease?
Prevention of different types of prostatitis like any other disease, healthy lifestyle, no bad habits and a balanced diet. If you have been diagnosed with prostatitis, exercise should not be neglected either. In the event of any reduction in inflammation, seek medical attention immediately to eliminate the cause and prevent the infection from spreading to other organs.
You should lead a decent lifestyle, have regular sex with your regular partner. It is important not to forget about personal hygiene of the genitals and not to neglect regular preventive examinations by a urologist. If a man knows what prostatitis can be and at the same time pursues a passive lifestyle, exercises should be performed to prevent congestion from appearing in the small pelvis.
To summarize
Depending on the causes and characteristics of the course, acute and chronic types of prostatitis are diagnosed. Chronic pelvic pain syndrome belongs to a separate group. Acute prostatitis is characterized by clinical manifestations such as chills, fever, and pain. The chronic form cannot manifest in any way or has a mild picture: urinary incontinence, painful pain in the pelvic area, which can lead to impotence and loss of fertility with the development of complications.
Acute prostatitis develops suddenly and is easily diagnosed. In contrast, chronic prostatitis progresses in waves, alternating periods of remission and exacerbation. In a chronic course, the identification of pathogenic microbes can cause some difficulties. Focal foci of infection in the urogenital system cause complications in the form of diseases of organs anatomically adjacent to the prostate gland. Depending on which prostatitis has been diagnosed, the urologist will prescribe a differentiated treatment regimen.




































